
Background: The manufacturing of customized prostheses is made possible by 3D printing, which welcomes in a new age of customization in dentistry by moving the field from manual to digital. Aims: To examine at how 3D printers have been used in dentistry manufacturing during the last ten years, looking at methodological methods, publishing trends, how dental prosthesis are distributed, how effective they and how satisfied patients are. Furthermore, to assess the precision and challenges of prosthesis fit in dentistry utilizing 3D printing technology. Methodology: Using the PubMed database, a systematic literature review of the literature investigated the use of 3D printing in dental practices from 2019 to 2024. Results: The overview shows a ten-year peak in dental 3D printing research, with publications tripling between 2020 and 2022 and then abruptly declining in 2024. Numerous uses, technology, prosthetic types, patient satisfaction, fit accuracy, and problems are all explored in studies. Interestingly, crown studies predominate, and SLA is the most often used printing technique. Overall, patient satisfaction is high, although there are some drawbacks, including as fitting problems and maintenance needs. Scientific Novelty: The creative use of 3D printing in dentistry improves the creation of customized dental prosthesis and transforms conventional manufacturing techniques. Conclusion: In conclusion up, 3D printing in dentistry holds potential for both surgical guiding and prosthesis manufacture.
Copyright © 2024 Maryan Domysche, Serhii Terekhov, Olena Astapenko, Stanislav Vefelev and Olha Tatarina. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
he dentistry industry is undergoing a significant transformation, propelled by the integration of cutting-edge tools, techniques, and technology, leading to a noticeable transition from manual to digital procedures. Over the past 10 years, the creation of new innovative, completely automated and accelerated prototyping methods has revolutionized the way in which three-dimensional dental prostheses are designed and made. The presented change must be incorporated within restorative dentistry to ensure that the field harmonizes with state-of-the-art approaches. Simultaneously, it is valid to state the added value which the conducted research makes to the already existing body of knowledge [1].
The advancement of computer-aided design and computer-aided manufacturing technologies has led to substantial progress in the field of digital dentistry, enabling it to effectively address a wide range of clinical challenges [2].
In the field of dentistry, the use of 3D printing technology provides an opportunity for the fabrication of personalized components and prostheses and in this way bring the new changes traditional manufacturing approaches. The technological advancement artificial intelligence, machine learning, and image identification addresses healthcare concerns and promote innovative solutions for effective and efficient treatment [3]. Globalization and the digitization also affect the economic by making prosthesis cost effective. To encounter such challenges needs innovations for specialized training and utilization of financial resources. It is necessary for all stakeholders to collaborate and apply transformative potential of this technology [4]. Research and education are also affected by AI, trajectory of technology and digitalization. The research revealed a lot of challenges related to the integration of technology like shortages in talent and concerns related to ethics [5]. Currently, digitalization particularly technological advancement plays a crucial role in shaping the worldwide financial markets, promoting effectiveness, and creating opportunities for innovative solutions [6].
The advanced technologies like artificial intelligence machine learning, and image identification have the potential to enhance the 3D printing technique employed in the production of dental prostheses and components. The prostheses accuracy is closely associated with enhanced therapeutic outcomes like improved fit, durability, and patient satisfaction [7]. In spite of the widely use of advance dental CAD/CAM systems, there is still a lack of research on instrumental assistance for dental prosthetic. There is a need to incorporates artificial intelligence, machine learning and 3D printing technologies to enhance the efficiency, precision, and competitiveness of dental prosthetic production procedures [8]. Furthermore, this research proposes the use of circular economy ideas, incorporating sustainable practices and leveraging research and development efforts in 3D printing technology, to reduce production costs while simultaneously promoting environmental sustainability [9].
Among the latest advancements is three-dimensional printing, an additive manufacturing method that has become integral to modern dental practices [10]. Many dental treatment fields, such as orthodontics, dental implants, mandibular reconstructions, prosthodontic rehabilitation, and both surgical and nonsurgical endodontics, make substantial use of this technology [11]. For nearly three decades, 3D printing technologies have stood as advanced manufacturing methods, leveraging computer-aided design digital models to automatically produce personalized 3D objects. Widely embraced in industries spanning from design and engineering to manufacturing, these technologies offer a multitude of advantages in process engineering. Their applications in dentistry are found in many different fields, such as orthodontics, endodontics, prosthodontics, oral and maxillofacial surgery, and oral implantology [12]. The study on European countries’ response to the COVID-19 pandemic revealed distinct clusters based on healthcare preparedness. Recommendations for improving response strategies include educational campaigns on vaccination importance and bolstering healthcare staff and infrastructure. 3D printers in the field of dental production present optimistic opportunities for creating customized dental prostheses and components, hence improving accuracy and personalization in dental treatment. The potential benefits of incorporating 3D printing technology into dental operations include the optimization of production processes and the provision of customized dental solutions, ultimately leading to enhanced patient care and improved treatment outcomes [13]. The implementation of color teaching approaches can greatly enhance memory retention and cognitive engagement, as demonstrated by the inclination of medical students to employ color coding when studying humanities that has the potential to improve instructional materials in other domains, such as the utilization of 3D printing in dental prosthesis and components production [14].
The field of additive manufacturing, which is also known as 3D printing, has advanced to the point that it can manufacture intricate and valuable final products, beyond the requirement for rudimentary prototypes. This further enable dental professionals to promptly enhance and modify prosthetic designs in response to patient input and clinical assessments. The benefits of utilization of this improves operational cost, effectiveness and time saving [15]. In the field of oral and maxillofacial surgery this 3D printing technology is extensively utilized for the sequential creation of objects through the utilization of digital models as a guide and have the ability to print materials, suitable for therapeutic applications in dentistry [16]. Research have also shown that 3D-printed dental prostheses in clinical settings yield a successful outcome in terms of conformity, comfort, and visual appeal, and overcome the constraints of traditional denture manufacturing methods for patients [17]. In addition, tis further help dental teams to accurately strategize and carry out complex surgical operations, enhancing both the practical and visual results for patients through the utilization of sophisticated imaging techniques and computer-aided design/computer-aided manufacturing software, [18]. There are not only benefits and significant potential, but there are certain challenges, including cost constraints, regulatory considerations, and technical limitations. A collaboration between dental professionals, researchers, manufacturers, and regulatory agencies is required to ensure the safe and effective integration of 3D printing technology in clinical work [19]. Looking ahead, future developments in 3D printing hardware, software, and materials are poised to further enhance its capabilities in dental prosthetics. From the emergence of novel bioresorbable materials to advancements in intraoral scanning and digital impression techniques, ongoing innovation holds the promise of expanding the scope and efficacy of 3D-printed dental solutions [20, 21]. In summary, the use of 3D printers in dentistry manufacturing practice is a revolutionary development in the prosthetics industry. With its unmatched accuracy and speed, 3D printing technology makes it possible to fabricate customized prosthetic components and devices, which has the potential to transform the provision of oral healthcare and enhance patient outcomes. Future dental technology is expected to be significantly shaped by 3D printing as study into its potential and solutions for current issues continues. Research objectives are following,
To investigate the trends and shifting dynamics of publication counts of the use of 3D printers in dentistry manufacturing during the previous ten years.
To assess the various methodological perspectives used in research on dental 3D printing.
To examine how different 3D printing technologies are distributed in relation to dental manufacturing practices.
Examine various types of dental prosthesis in order to determine the extent and direction of study on specific dental components made with 3D printing technology.
To assess patient satisfaction with 3D printing in dental treatment as well as the clinical effectiveness of dental materials and procedures.
To assess how well dental prosthesis fit, how snug they are, and what issues arise when employing 3D printing technology.
A systematic literature review approach to gather and analyze relevant literature on the use of 3D printers in dental production practice from 2019 to 2024.
Figure 1 illustrates a systematic literature search conducted on PubMed using keywords “3D printing” OR “Printing, Three-Dimensional” OR “Printing, Three-Dimensional/economics” OR “materials for 3D printing” OR “3D printing materials” AND “dentistry” OR “digital dental technology” OR “digital dentistry integration” OR “digital dentistry implementation” resulting in the identification of 3,475 publications. These publications were then screened based on inclusion and exclusion criteria, including the years 2019-2024, availability of free full text, language (English only), and focus on human subjects. After applying these criteria, 449 records were deemed eligible for assessment. From these, 37 highly relevant studies were included for further analysis, indicating a subset of literature specifically addressing the intersection of 3D printing technology in dental production practice for manufacturing individualized dental prostheses and elements within the specified timeframe and parameters.

The inclusion criteria for selecting studies from the systematic literature search conducted on PubMed using specific keywords included publications between 2019 and 2024, availability of free full text, English language publications, studies focusing on human subjects, and content directly addressing the utilization of 3D printing technology in dental production practice for manufacturing individualized dental prostheses and elements. Conversely, exclusion criteria comprised studies published outside the specified timeframe, publications without free full-text access, non-English language publications, studies not involving human subjects, and content unrelated to the application of 3D printing technology in dental production practice for manufacturing individualized dental prostheses and elements. This criterion was applied to ensure the selection of relevant literature related to the intersection of 3D printing technology and dental prosthetic production.
Figure 2 shows the result of current review. There was a significant upward surge in publication over the past decade. There were 121 publications in year 2015, and the trend shows steady growth, with acceleration from 2018 onwards. Result also shows a significant increase in publication counts, nearly doubling from 2020 to 2022 had a, indicating an escalation in scholarly activity or an expansion of the discipline. In addition to these results also shows an abrupt decrease in year 2024, which suggesting a change in research emphasis, alterations in methodology, or external influences impacting publishing rates.
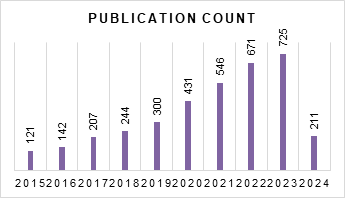
Table 1 illustrates study characteristics included in current review from2019 and 2024, examining the application of 3D printers in the field of dental manufacturing. Result shows a range of study designs, such as experimental studies, cohort studies, clinical studies, comparative studies, systematic reviews, in vitro studies, and cross-sectional studies and reflects a multidisciplinary approach to comprehending the applications and implications of 3D printing in the field of dentistry. As far Sample sizes are concerned, these are varied significantly across studies, ranging from small-scale experiments with as few as three participants to larger cohort sizes exceeding 200 individuals, reflecting the diverse scopes and methodologies of the research conducted. The majority of the studies included in this review focus on recent advancements, highlighting the ongoing relevance and evolving nature of research related to 3D printing.
| Author’s | Publication Year | Study Design | Sample Size |
| Temizci et al. [22] | 2024 | Experimental study | 200 |
| Zhu et al. [23] | 2024 | 18 | |
| Choi et al. [24] | 2024 | 36 | |
| Rosentritt et al. [25] | 2023 | 58 | |
| Altarazi et al. [26] | 2022 | 147 | |
| Ohara et al. [27] | 2022 | 23 | |
| Ottoni et al. [28] | 2022 | 30 | |
| Chevalier et al. [29] | 2022 | 108 | |
| Cresswell-Boyes et al. [30] | 2022 | 34 | |
| Srinivasan et al. [31] | 2021 | 15 | |
| Srinivasan et al. [32] | 2021 | 25 | |
| Lee et al. [33] | 2021 | 5 | |
| Held et al. [34] | 2021 | 34 | |
| Kim et al. [35] | 2020 | 16 | |
| Metlerski et al. [36] | 2020 | 10 | |
| Saadi et al. [37] | 2023 | 32 | |
| Parakaw et al. [38] | 2023 | 3 | |
| Bjelopavlovic et al. [39] | 2024 | Cohort Study | 21 |
| Petre et al. [40] | 2023 | 205 | |
| Panpisut et al. [41] | 2022 | 61 | |
| Suryajaya et al. [42] | 2021 | 35 | |
| Park et al. [43] | 2019 | 20 | |
| Hou et al. [44] | 2024 | Clinical Study | 260 |
| Ding et al. [45] | 2023 | 55 | |
| Khan et al. [46] | 2024 | In vitro study | 36 |
| Farag et al. [47] | 2024 | 60 | |
| Hajjaj et al. [48] | 2024 | 60 | |
| Kim et al. [49] | 2023 | 160 | |
| Kwon et al. [50] | 2021 | 20 | |
| Frąckiewicz et al. [51] | 2024 | Systematic Review | 686 |
| Al-Makramani et al. [52] | 2023 | Comparative Study | 10 |
| Refaie et al. [53] | 2023 | 20 | |
| Paradowska-Stolarz et al. [54] | 2023 | 10 | |
| Reis et al. [55] | 2020 | 8 | |
| Karatekin et al. [56] | 2019 | 40 | |
| Curinga et al. [57] | 2023 | Cross-Sectional Study | 15 |
| Hegedus et al. [58] | 2022 | 120 |
Table 2 provides a comprehensive overview of the distribution of various 3D printing technologies within the context of dental production practice, as identified in a systematic literature review. Stereolithography emerges as the most frequently mentioned technology, cited in seven instances across multiple studies [22, 25, 26, 40, 45, 47, 52]. Digital Light Processing follows with four mentions [22, 30, 35, 50], while Fused Deposition Modeling and resin-based 3D printing each appear twice [36] and [41] respectively. Additionally, the review encompasses a diverse range of other 3D printing technologies, collectively referenced 21 times [23, 26, 27, 28, 29, 30, 31, 32, 33, 34, 37, 38, 40, 41, 43, 48, 49, 53, 55, 57, 58]. This comprehensive overview underscores the multifaceted application of 3D printing in dental prosthetic and element manufacturing, providing valuable insights into the evolving landscape of dental production technologies.
| 3D Printing Technology | Frequency | Author’s |
| Stereolithography (SLA) | 7 | [22, 25, 26, 40, 45, 47, 52] |
| Digital Light Processing (DLP) | 4 | [22, 30, 35, 50] |
| Fused Deposition Modeling (FDM) | 2 | [36, 44] |
| Resin-based 3D printing | 2 | [41, 46] |
| Various 3D printing technologies | 21 | [23, 26,27,28,29,30,31,32,33,34, 37, 38, 40, 41, 43, 48, 49, 53, 55, 57, 58] |
Table 3 shows the categorizes of various types of dental prostheses discussed in the reviewed studies. It outlines five main categories: Crown and Restoration Studies, Implant and Surgical Guides, Denture Studies, Partial Dentures and Edentulous Models, and Miscellaneous Dental Prostheses. Crown and Restoration Studies, focusing on the development or evaluation of crowns and restorations, were the most frequently discussed, with 12 studies cited [22, 27, 28, 29]. Following this, Implant and Surgical Guides, Denture Studies, and Partial Dentures and Edentulous Models were also represented, with 6 [23, 39, 43, 44, 48, 58], 3 [24, 26, 33], and 4 [31, 32, 38, 57] studies respectively. Additionally, a category termed Miscellaneous Dental Prostheses covered various aspects not fitting into the other categories, including wear resistance, digital dental models, and tooth replicas, among others, with 12 studies included [25, 29, 30, 34, 36, 37, 40, 41, 42, 45, 52, 56]. Each entry in the table provides details such as the author(s) and publication year of the cited study, offering a comprehensive overview of the literature on the utilization of 3D printers in dental production and the specific types of dental prostheses explored in the reviewed studies.
| Dental Prosthesis Type | Description | Frequency | Author’s |
| Crown and Restoration Studies |
Studies related to the development or
evaluation of crowns and restorations. |
12 | [22, 27,28,29, 35, 47, 49,50,51, 53,54,55] |
| Implant and Surgical Guides |
Studies focusing on the development or
utilization of guides for implant placement or surgical procedures. |
6 | [23, 39, 43, 44, 48, 58] |
| Denture Studies |
Studies related to the development or
assessment of dentures. |
3 | [24, 26, 33] |
| Partial Dentures and Edentulous Models |
Studies focusing on partial dentures or
models of edentulous areas. |
4 | [31, 32, 38, 57] |
| Miscellaneous Dental Prostheses |
Studies covering various aspects not
primarily categorized into other types, including wear resistance, digital dental models, simulated dental models, tooth replicas, etc. |
12 | [25, 29, 30, 34, 36, 37, 40,41,42, 45, 52, 56] |
Table 4 provides a comprehensive overview of results that encompass the clinical effectiveness of dental materials and techniques, the utilization of 3D printing and CAD/CAM in dentistry, the assessment of dental restorations and prosthetics, the evaluation of implantology techniques and procedures, and the assessment of orthodontic and surgical applications. Most commonly appearing studies within these categories include 3D printing and CAD/CAM applications [23, 36, 38, 52, 58]; dental restorations and prosthetics [31, 33, 46, 49, 53,] and the evaluation of orthodontic and surgical applications [34, 35, 41, 43, 50,]. This summary provides a significant perspective on contemporary research and clinical methodologies, benefiting academics, practitioners, and stakeholders.
| Clinical Efficacy | Description | Frequency | Author’s |
| Evaluation of Dental Materials and Techniques |
Evaluate different dental materials and treatments, in terms of strength,
hardness, ability to remove biofilm, resistance to wear, and marginal fit. |
8 | [22, 24, 25, 37, 44, 45, 47, 48] |
| 3D Printing and CAD/CAM Applications in Dentistry |
Evaluate the many applications of 3D printing and computer-aided
design/computer-aided manufacturing technologies within the field of dentistry in terms of utilization, implants, restorations, and surgical guidance. |
5 | [23, 36, 38, 52, 58] |
| Evaluation of Dental Restorations and Prosthetics |
Clinical effectiveness of dental restorations and prosthetic devices, in
terms of key aspects such as marginal adaption, internal fit, and survival rates. |
5 | [31, 33, 46, 49, 53] |
| Assessment of Implantology Techniques and Procedures |
Evaluate the efficacy of diverse methodologies and protocols in terms
of decontamination approaches, marginal fit e, adaptation, and the rates of implant survival and restorations. |
7 | [26,27,28,29, 32, 39, 57] |
| Evaluation of Orthodontic and Surgical Applications |
To assess the various applications of orthodontics and surgery,
including processes such as cavity preparation, diagnostics, treatment planning, periodontal regeneration, toxicity reduction in radiation therapy, and the precision of surgical procedures utilizing computer- aided design and computer-aided manufacturing technology. |
6 | [34, 35, 41, 43, 50, 54] |
Table 5 presents a comprehensive overview of patient satisfaction across different dimensions concerning the implementation of 3D printing technology in dental care. The table categorizes patient satisfaction into three main themes: Knowledge and Abilities Enhancement, Treatment Outcome Satisfaction, and General Satisfaction Metrics. Under Knowledge and Abilities Enhancement, [39] reported a single instance of satisfaction. In the Treatment Outcome Satisfaction category [40, 44, 49, 52] collectively contributed four instances of satisfaction. General Satisfaction Metrics included [27], accounting for three instances of satisfaction. Additionally, single instances of satisfaction were reported for Patient-Reported Outcomes [34], and Accuracy and Precision, examined [55]. This table succinctly summarizes the varied dimensions of patient satisfaction regarding the application of 3D printing in dental practice, offering valuable insights into its effectiveness and acceptance among patients.
| Patient Satisfaction | Frequency | Author’s |
| Knowledge and Abilities Enhancement | 1 | [39] |
| Treatment Outcome Satisfaction | 4 | [40, 44, 49, 52] |
| General Satisfaction Metrics | 3 | [27, 31, 4] |
| Patient-Reported Outcomes | 1 | [34] |
| Accuracy and Precision | 1 | [55] |
Table 6 synthesizes findings from a systematic literature review on the utilization of 3D printers in dental production practice, specifically focusing on the accuracy and snugness of prosthetic fit. Bjelopavlovic et al. 2024 [39] highlight the value of individualized models, with 81% of respondents finding them valuable. Farag et al. 2024 [47] and Refaie et al 2023 [53] evaluate prosthetic fit through various measurements, while Curinga et al. 2023 [], Petre et al. 2023 [40], Ottoni et al. 2022 [28], and Kim et al. 2020 [35] present diverse measurement results indicating different aspects of fit, such as potential impact due to linear distortions in tooth dimensions and acceptable ranges of marginal and internal gaps. Srinivasan et al. 2021 [31] find no significant difference in fit between milled and 3D-printed CRDPs, while Held et al. 2021 [34]emphasize tailoring prostheses to individual patients and treatment intentions. This synthesis offers insights into the current state of prosthetic fit accuracy and snugness within the realm of 3D printing in dental prosthetics.
| Prosthetic Fit | Description | Frequency | Author’s |
|
Value of Individualized
Models |
81% found individualized models valuable | 1 | [39] |
| Evaluation Method |
Evaluated through marginal discrepancy
measurements; Evaluated through marginal gap and internal fit measurements |
2 | [47, 53] |
| Measurement Results |
Indicated potential impact on fit due to linear
distortions in tooth dimensions; Satisfactory; Smaller gap thickness at the occlusal region for 3D-printing/pressed crowns; Marginal and internal gaps measured, found within acceptable range |
4 | [28, 35, 40, 57] |
|
Comparison of
Manufacturing Methods |
No significant difference in fit between milled
and 3D-printed CRDPs |
1 | [31] |
|
Tailoring to Patient and
Treatment Intention |
Tailored to the individual patient and treatment
intention |
1 | [34] |
Table 7 presents a compilation of complications associated with the utilization of 3D printers in dental production practice.
| Complications | Author’s |
|
3D-printed casts showed poorer fit
compared to alginate-derived casts |
[52] |
| Minimal | [40] |
|
Failure modes included radial cracks
and cone cracks |
[28] |
|
3D-printed CRDPs required more
maintenance visits, adjustment time, and adjustment costs |
[31] |
|
Acute radiation-induced oral mucositis,
other treatment-related toxicities |
[34] |
Al-Makramani et al. 2023 [52] reported poorer fit of 3D-printed casts compared to alginate-derived casts. Petre et al. 2023 [40] noted minimal complications, while Ottoni et al. 2022 [28] observed failure modes such as radial cracks and cone cracks. Srinivasan et al. 2021 revealed that 3D-printed CRDPs necessitated a greater number of maintenance visits, adjustment time, and adjustment expenses in comparison to conventional approaches [31]. In a study conducted by Held et al. (2021), acute radiation-induced oral mucositis and other treatment-related toxicities were reported [34].
Current study spanning from 2019 to 2024 period reveals a dynamic and fast changing research environment regarding the utilization of 3D printing in dental settings, and seeks to investigate multiple facets including clinical effectiveness, material characteristics, and production techniques. Rising publication in this field indicates ongoing progress and emphasizes the enduring significance of 3D printing. This exemplifies the dynamic progression of 3D printing research in the field of dentistry, showcasing an ongoing quest for knowledge and advancement. Similarly, another systematic focused on a qualitative examination of published research on the therapeutic application of restorative material 3D printing using stereolithography. Stereolithography-based 3D printing is growing at a quick pace, which is indicative of major technological advancement with a great deal of disruptive potential. Dentistry has demonstrated an amazing openness to modifying procedures, materials, and techniques to accommodate this exciting new digital technology [59]. However, there are a few clinical barriers that prevent functional part manufacture using 3D printing, including dimensional accuracy, wear resistance, wet strength, and aesthetic appearance. The dearth of clinical trials and reporting on definitive/permanent dental restorative materials and structures may be explained by these restrictions. Additionally, a different literature study investigates the various methods used by modern 3D printers and how they are used to printed dental materials. Another research indicates that the use of 3D printing makes it simpler for dentists to implement various additive manufacturing processes, which in turn improves workflows and results in clinical outcomes that are more satisfactory [50].
The Current review also have stressed the widespread adoption of stereolithography and digital light processing in the field of dental fabrication, because of their remarkable accuracy and suitability for complex prosthetic procedures in dentistry demonstrating their effectiveness and dependability. While possibly because of limitations in resolution or materials alternative methods like fused deposition modeling and resin-based procedures are less common. Furthermore, another study examines the influence of social media on the acceptance of 3D printing technology within the dentistry profession and reveal the extensive adoption of 3D printers, especially among dentists and dental workers. The individual having an average career experience of 3.8 years, possess an average of 3.6 printers per individual emphasizing the importance of digital professional networks in promoting knowledge sharing and supporting innovation in the field of dental 3D printing [61]. Moreover, the latest progress in additive manufacturing and imaging technology has introduced a new age in the field of clinical dentistry by creating opportunities for new possibilities, resulting in promising results. These innovations have a significant impact on enhancing patient care and treatment methods in dentistry [62].
The current study also has emphasized on crown and restoration within dental practices, showing a significant interest in the role of 3D printing and highlights a growing focus on Implant and surgical guides, in precision for procedures. However, the current study also shows that there is a relative lack of research concerning denture studies and partial dentures, creating a room for further investigation. The miscellaneous dental prostheses category underscores the diverse applications of 3D printing in dentistry, hinting at its potential to revolutionize various aspects of dental care. Similarly another study focusing on biomaterials, fabrication techniques, clinical performance, and patient satisfaction with predominant use of CAD/CAM technologies shows that 3D printing is primarily utilized for custom trays, interim, and immediate dentures due to limitations in esthetics, retention, and occlusion [63]. Similarly, another review explores the advancements in 3D printing technologies for dental prosthetics and review the details of various techniques, materials, and applications, highlighting the potential of additive manufacturing to swiftly produce complex dental structures. With this offers dentists greater flexibility and efficiency in their practice [64]. Current study is delving into various aspects of dental materials, techniques, and technologies such as 3D printing and CAD/CAM and emphasis on evaluating the clinical performance of restorations, prosthetics, and implantology techniques to ensure better patient care in dentistry practices. Furthermore, this research also integrated the orthodontic and surgical studies, reflecting in a multidisciplinary approach to tackling clinical challenges effectively. Similarly, another study conducted to evaluate the precision of occlusal devices created using CAD/CAM technology, including variations in vertical heights (2.5 mm and 4.5 mm) and revealed that devices with reduced height exhibited superior accuracy. The devices exhibited large variations in trueness and precision values, with only slight variances in volume detected [65]. Another study examined the practical use of CAD/CAM and 3D printed dentures in clinical settings emphasized the benefits of these technologies, including time efficiency, enhanced clinical results, and the protection of patient records. Although computerized dentures show potential, they still necessitate clinical try-ins to provide the best outcomes. Moreover, it is imperative to acknowledge the constraints associated with the use of computerized dentures especially associated cost [66].
Patient satisfaction with the use of 3 D printing technology is another important concern. The current study has explored the complex terrain of patient satisfaction pertaining to the use of 3D printing technology in the field of dentistry taking into account variables such as therapy results, advancements in knowledge, overall satisfaction measurements, outcomes stated by patients, and precision of procedures. Patients shows different viewpoints regarding the benefits of 3D printing in dentistry with varying degrees of satisfaction across these parameters. A multitude of research have made significant contributions and demonstrating a persistent interest in understanding patient happiness and enhancing the usage of 3D printing technology in the realm of dental treatment and play a crucial role in customizing strategies to effectively satisfy the expectations of patients. Similarly , another thorough evaluation highlights the benefits of resin 3D printers in the field of dentistry and revealed that these printers provide exceptional accuracy, extensive customization choices, efficient time management, cost reduction, greater patient satisfaction, improved communication, and a diverse range of appropriate materials [67]. Furthermore, an empirical investigation on the durability of milled zirconia restorations in comparison to 3D-printed resin restorations indicate that 3D-printed resins have the potential to be a feasible substitute for milled zirconia, especially in the context of creating novel biocompatible materials [68]. Furthermore, another study examine the level of accuracy and precision exhibited by various types of 3D printers and shows that DLP printers demonstrate a higher degree of accuracy in the manufacturing of dental models when compared to LCD printers highlighting the crucial role of choosing suitable printing technologies to attain the best possible results [69].
During last ten years, the use of 3D printing in dentistry has resulted in a substantial shift in treatment approaches and has facilitated the creation of automated and customized treatment plans, resulting in the efficient and cost-effective production of precise dental devices leading to enhancements in patient care. Current study also emphasized on the implications of prosthetic fit within dental production, particularly in the context of 3D printing and indicate a positive trend towards personalized models, with a range of assessment methods employed, such as marginal discrepancy and internal fit evaluations. Interestingly, comparisons between traditional milling techniques and 3D printing methods. Similarly other relevant research also show that the advancements in accuracy achieved through tailored approaches and advanced manufacturing techniques are promising and evident that further research and standardization efforts are necessary to fully optimize prosthetic outcomes in dental practice [70]. Furthermore, there’s a growing body of literature encompasses various prosthetic restorations, including implants and innovative implant-scaffolds. This widespread adoption of dentistry 4.0 further emphasized the need for aligning dental practices with holistic Industry 4.0 models, highlighting the advantages and necessity of such integration [71]. Moreover the increasing use of 3D printing in dentistry is most focused important area that is being examined now a days because of the ability to personalize and customize dental items made possible by this technology [72].
The current study also highlights several issues on dental 3D printing including higher maintenance requirements, treatment-related adverse effects such oral mucositis, and structural flaws in prosthetics. Notably, problems with printed models such as radial and cone cracks point to possible durability issues, while implementation hurdles include additional maintenance visits and adjusting expenses. All these result shows how crucial it is to continue research and development in dental 3D printing in order to provide better patient care and results. These results are in line with other research that emphasizes how important it is for 3D printing technology to progress for dental applications and have shown that 3D-printed teeth have some benefits over actual teeth; nonetheless, there are still issues, especially with resin hardness and printing canal architecture accurately [73]. Another study highlights the concerns about the layer-by-layer superposition principle in 3D printing, resulting in anisotropy, leading to varying mechanical properties in different directions. This variability could affect the long-term durability of intraoral prostheses. [74]. Moreover, research on the difficulties in integrating 3D printing into dental offices finds that dentists, technicians, and 3D printing firms all lack awareness of the main barrier. It is imperative that personnel be trained, and that this knowledge gap be closed, particularly in light of the widespread inclination toward conventional approaches. The fact that investment costs are not listed as the main worry is surprising and highlights the need to close knowledge gaps in order to fully reap the benefits of additive manufacturing in dentistry [19]. There should be training and development programs for dental practitioners to provide efficient and effective dental care.
In summary, current review on the use of 3D printers in dentistry indicates a quickly changing field that is marked by technical developments and interdisciplinary research and indicates that 3D printing has great potential to transform many facets of dental treatment, especially surgical guiding and prosthesis manufacturing.
Digital light processing and stereolithography are among the two most popular methods and are incredibly precise for complex dental work in spite of the issues with wear resistance, dimensional correctness, and aesthetic appeal continue to prevent 3D-printed restorations from being widely used.
Current review also emphasized that there hasn’t been much done in this field, which indicates that targeted exploration is needed on priority basis. Subsequent research should focus on creating novel materials especially designed for denture construction, with an emphasis on heightened durability and improved visual attributes to provide quality of care to the patient. Continuous research on comparing the lifetime of 3D-printed restorations to conventional techniques will also provide an important insight on the dependability and endurance of the dental prostheses. Moreover, comparison must also be done, in order to answer the various viewpoints on patient satisfaction, patient experiences and preferences.
Resin 3D printing technology has the potential to revolutionize dental offices because it offers a great precision, customization choices, and cost reductions. Biocompatibility, mechanical characteristics, and aesthetic results like aspects should be the focus of future research.
In conclusion, even if research to far highlights the revolutionary potential of 3D printing in dentistry, there are still a lot of opportunities for development and research. Through the implementation of focused research approaches and the resolution of recognized obstacles, the dentistry community may fully use the potential of 3D printing technology to improve treatment outcomes and patient care.
Standardization efforts and training programs are much more important for the successful use of 3D printing technology in the dentistry field. For this, it is necessary to create certain frameworks or norms that standardize dental clinics’ 3D printing procedures like material selection, printing specifications, post-processing methods, and quality control procedures. Furthermore, to fulfill the knowledge gap it is also compulsory to create specialized educational programs, create seminars or certifications that offer theoretical and practical instruction on 3D printing materials and techniques. These training activities and courses must address things like design optimization for dental applications, comprehending the characteristics of various printing media, and resolving typical printing-related problems. Intersectoral coordination like partnerships with academic institutions, professional groups, and technology suppliers can be formed to successfully implement these instructional programs. Academic institutions also put their experience in developing the educational curricula and training and development, while collaborating with IT companies can give access to state-of-the-art printing hardware and software. In order to support dental practitioners’ chances for continuous education and to advocate for standardized procedures, professional groups can be extremely important. Through partnerships and large-scale educational program investments, the dentistry community may improve its capacity to use 3D printing technology efficiently. This strategy will promote innovation and improvement in dental manufacturing techniques in addition to ensuring improved patient care results.